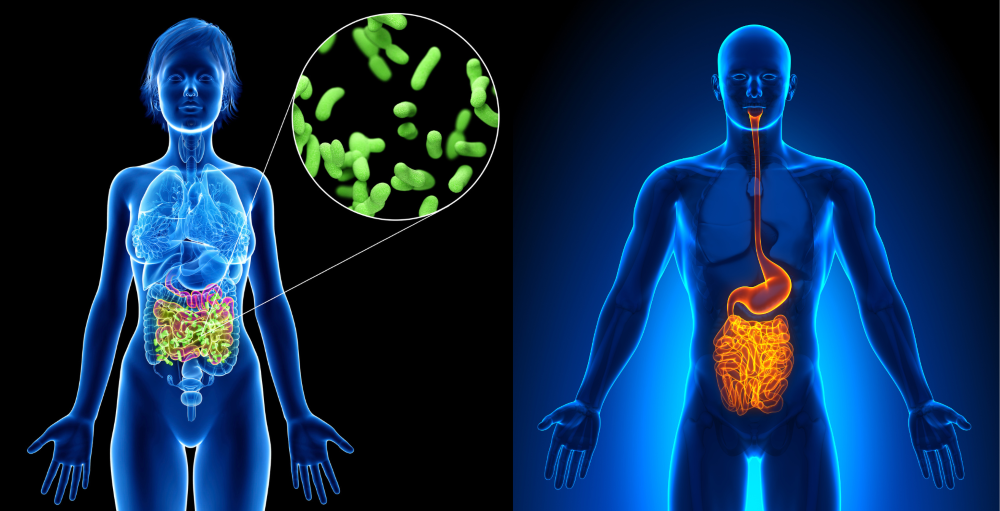
What is a gut microbiome
The bacteria that live within the human colon (or large intestine) are known as the gut microbiota – more recently termed the gut microbiome.
It is thought that tens of trillions of microorganisms are present in this microbiome – including at least 1000 different species of known bacteria. This complex ecosystem develops as a result of interaction between the host and the bacteria that are introduced from the environment soon after birth.
Studies suggest that each person has their own distinct microbial make-up that remains relatively constant once adulthood is reached, however, the composition of the microbiome may alter as a result of environmental factors such as diet and antibiotic usage.
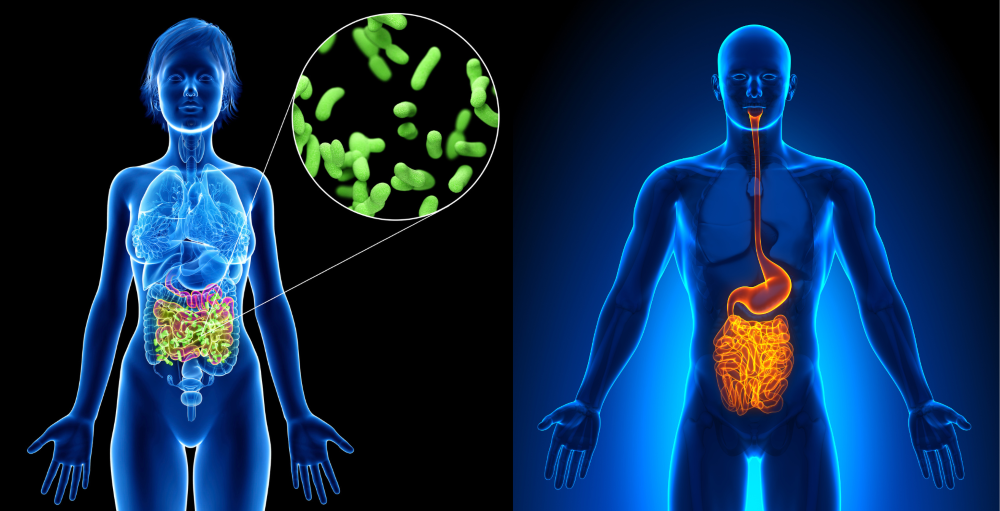
What does the gut microbiome do
The microbiome performs a variety of functions that are essential to health, such as:
- maintaining the inner lining of the intestines,
- digestion of food and
- provision of nutrients and vitamins.
The microbiome can protect against pathogens (disease-causing bacteria and viruses) and also play a key role in the proper functioning of the immune system.
However, the gut microbiome has also been implicated in the development of many conditions from irritable bowel syndrome to obesity. More recently, it is thought that variations in the composition of the gut microbiome may be involved in the development of colorectal cancer.
How may the gut microbiome cause colorectal cancer?
The exact mechanisms have not been conclusively identified.
It is thought that some bacterial by-products promote a toxic environment within the colon, and that some bacteria themselves can release toxins. It is also thought that some bacterial species lead to a pro-inflammatory environment that initiates and promotes DNA mutations in our cells that lead to tumour formation.
How do researchers know what bacteria are in someone’s microbiome?
Earlier studies involved taking an individual’s faeces and using culturing techniques to grow the colonic microbiota.
We now know that this is inaccurate, as the majority of the bacteria living within the colon are called “obligate anaerobes”. This means that they can only grow successfully in the absence of oxygen. This meant that culturing techniques preferentially selected out the bacteria that were able to grow in an oxygenated atmosphere.
More recently, molecular techniques have been used on faecal samples. Techniques can now identify the bacteria based on their DNA, without any need to try and grow them. In 2008, the US National Institute Of Health launched the Human Microbiome project whose aim was to characterise the human microbiome at 5 sites – the colon being one of them. The project utilised stool samples for over 200 healthy subjects and used the DNA techniques. Results published in 2012 showed an enormous amount of variation in microbiome composition, even among healthy volunteers.
How can I find out more about my own microbiome?
There are now numerous commercial kits available that offer analysis of your own personal gut microbiome. These offer people the chance to send a stool sample for analysis.
Depending on the kit, results can detail the composition of the microbiome, including relative proportions of “good” and potentially pathogenic species, as well as species capable of causing potential gut inflammation.
Other analyses include how well your microbiome utilises fibre, and how your microbiome may be contributing to or lowering your risk of diseases such as heart disease or diabetes.
Why should I want to know this?
One major reason is that by knowing the types of bacteria in your microbiome, you can start to make dietary and lifestyle changes to alter potential imbalances and promote a healthier gut.
For example, by increasing the amount of fibre in your diet, can encourage the growth of butyrate-producing bacteria – a short chain fatty acid that is known to promote gut health. This, along with other lifestyle changes may lower your risk of developing colorectal cancer and other bowel conditions.
Here at ROC Clinic we utilise such kits in order to help patients test their microbiome and work with them to develop an individualised plan to help improve their gut health.
Look out for our next blog where more information shall follow!
Want to discuss concerns about your gut microbiome? Get an appointment with one of our doctors!